“What are the statistics on homelessness and mental health in Toronto?”
This question came to us anonymously through our latest survey.
Over the years, the Homeless Hub blog series has written extensively on the links between mental health and homelessness in Canada, however, we’ve not yet focused on any specific location. As Canada’s largest and most ethnically diverse city, Toronto has the greatest number of people experiencing homelessness with 5,253 people counted on the 2013 Street Needs Assessment (SNA). The Toronto count in 2013 found that 79% of those surveyed were staying in shelters, 8% on the street, 6% in correctional facilities, 3% in violence against women (VAW) shelters, and 4% in health care or treatment facilities. A study on health care access for homeless people found that among Toronto’s homeless population, one third identified as an immigrant, 45% identified as belonging to a racialized group, 22% identified as Black and 9% as Indigenous.
Toronto’s SNA is used to estimate the number of people experiencing homelessness staying outdoors, or in a number of facilities on any given night. While the SNA offers important information, it does not provide an exact number of people experiencing homelessness in a community. For example, those disconnected from agencies serving the homeless population or who are couch surfing are likely not to be counted. However, a point-in-time estimate, such as Toronto’s SNA, does yield important information that would otherwise not be known.
Back in 2013, Isaac Coplan wrote a blog entry highlighting some of the findings in Toronto’s latest SNA, and I revisited the report to compile some data in connection to mental health, along with other statistics found in two other Toronto-focused studies on health and homelessness.
Mental Health & Homelessness in Toronto
The 2013 SNA highlights that 43% of respondents indicated that addressing their health needs was important. While only 2% indicated that mental health supports was most important to finding housing, 32% of respondents expressed an increased need for mental health services. Those who have been homeless for 2 years or more were two times more likely than those experiencing homelessness for a shorter period of time to indicate that mental health services was most important in finding housing. In contrast, 80% of women staying in VAW shelters indicated that help in addressing health needs was important to them, compared to 43% for all respondents. VAW shelter respondents were also 8% more likely to indicate the importance of mental health supports. Lastly, 49% of all respondents were on a subsidized housing waiting list and of those, 19% indicated having an application with the Coordinated Access to Supportive Housing system which provides access to housing catering to those with mental health and related needs.
While the 2013 SNA doesn’t provide further information beyond this data on mental health, it does provide a glimpse into the profile of homelessness in Toronto, and the rising needs for services required to better serve this population.
The Street Health Report 2007 reveals a similar picture of homelessness in Toronto based on a health survey for homeless adults in the downtown core. The findings in this study include:
- 35% of respondents had been diagnosed with at least one mental health condition in their lifetime.
- 12% said that they had mental health supports in the past but could no longer get help.
- The major reasons for not being able to obtain mental health care included:
- 38% did not have a doctor or didn’t know where to get care
- 29% saw a doctor but were not offered mental health care
- 24% were not able to get a referral to a specialist
- 24% did not have a health card
- 58% with a mental health diagnosis had been prescribed medication but:
- 28% said that the side effects were not explained to them
- 35% felt that they did not have a choice or say in their treatment plan
- 26% had been hospitalized with an average of 5 times for an emotional or mental health problem. Of this group:
- 70% said their most recent hospitalization was voluntary
- 30% were forced to go against their will
- 47% of respondents hospitalized in the past year of the study did not get help filling prescriptions when they were discharged from the hospital.
- 32% are unable to obtain medication due to the added expense, not having a benefit card or drug benefits not covering the prescription.
More recently, the Mental Health Commission of Canada conducted the At Home/Chez Soi study. The national study included demonstration sites in Vancouver, Winnipeg, Toronto, Montreal and Moncton and was the world’s largest trial of Housing First. The project aimed to develop evidence on effective services and interventions for people who are homeless and living with mental health conditions and ran from October 2009 to June 2013.
The Toronto participant sample covered a wide range of demographics: 68% were male, over 54% were between the ages of 35-54, 54% were born in Canada, 70% were single, 28% had children, 49% had less than high school education, 4% had prior military service and 95% were currently unemployed despite 68% having previously been employed for at least one year with the same employer. Findings from this group include:
- Of the 575 participants followed for two years, 67% met the criteria for two or more mental illnesses or addiction, of which 37% had a psychotic condition.
- 43% of participants had two or more hospital admissions for a mental illness in any one-year period in the five years before study entry.
- 5% of participants reported having been hospitalized for mental health at least once for more than 6 months in that time period.
- 30% reported symptoms consistent with moderate to high suicide risk.
Toronto has a large network of mental health services for individuals who are both housed and homeless including inpatient/outpatient services, case management, crisis programs and ethnoracial-focused agencies, yet there is a great need for an integrated approach to better serve this population. In our section on systems approach to homelessness, we emphasize the need to utilize an inter-agency collaboration, individualized programming and community-based service provision. The At Home/Chez Soi study demonstrated that with coordinated support systems under a Housing First framework, people who are homeless and have a mental health condition can live independently in the community, and the majority indicated that they would prefer to do so.
Overall, the mental health status of people experiencing homelessness in Toronto is alarming. Many report extremely high rates of mental health symptoms and suicidal ideation. However, it’s important to note that unlike the common stereotype of the homeless person suffering from psychosis, the most common conditions are depression and anxiety.
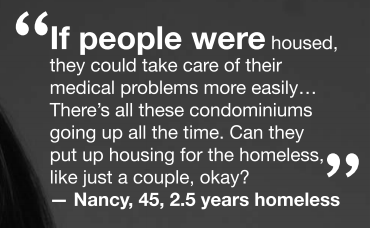
While quantitative methods reveal critical figures required for policy development that directly impact Canadians, people’s experiences and realities cannot be measured in numbers alone. Both The Street Health Report 2007 and the At Home/Chez Soi study used qualitative methods, including narrative interviews to reveal their experiences with mental health, homelessness, coping strategies and resilience. Qualitative data such as stories help us better understand the reality in unique ways that statistics simply cannot do.
Services in Toronto
With research increasing in the area of mental health and homelessness so are the programs available in Toronto, which include but are not limited to:
- Street Health is a non-profit agency providing physical and mental health programs in the Dundas and Sherbourne area. Their community mental health program supports people access health services and has nurse practitioners who provide care at their drop-in centres and shelters.
- Anishnawbe Health Toronto operates a 24/7 mental health crisis management service. They offer care from many disciplines including Traditional Healers, Elders and Medicine People, ancient ceremonies and traditions, intrinsic to Indigenous Peoples’ health care model.
- Sistering provides basic services to women who are homeless and under-housed. Among their services, they offer crisis intervention and prevention support for women dealing with trauma and abuse.
- Fostering an Inclusive Shelter Environment for LGBTQ2S Youth is a new mandatory training curriculum for Toronto’s shelters staff on topics of LGBTQ2S youth homelessness and the high rates of suicide and mental health.
- CATCH is a program offered by St. Michael’s Hospital, CAMH, and St. Joseph’s Health Centre designed for people experiencing homelessness and needing care. The program provides referrals to patients and remains connected with them to ensure that they are receiving the care they need.
While these are just a few initiatives, advocates call on the need to integrate mental health care and homeless services as featured in CAMH’s Nowhere to Go film that focuses on LGBTQ2S experiences in the shelter system. There are also gaps in the literature and further research is required to shed light on the experiences and needs of key populations through an intersectional framework. This would enable service providers and policy-makers to better understand the specific needs of homeless individuals living in Canada’s most diverse city.
More Toronto-Based Resources
- Racialised Groups and Health Status: A Literature Review Exploring Poverty, Housing, Race-Based Discrimination and Access to Health Care as Determinants of Health for Racialised Groups
- Guide to Services for People who are Homeless
- Living on the Ragged Edges: Latin Americans and Muslims and the Experience of Homelessness in Toronto
- Mental health and addictions: How Ontario and Toronto can improve lives while saving billions
- Learning from the Groundbreakers – Models of Innovation in Addressing Mental Health Equity in Toronto
Image Credit: The Street Health Report 2007 and 2013 Street Needs Assessment (SNA)