This post is part of our Friday “Ask the Hub” blog series. Have a homeless-related question you want answered? E-mail us at thehub@edu.yorku.ca and we will provide a research-based answer.
Dear Homeless Hub
Many times when I come across a person who appears to be homeless, he/she also seems to be mentally ill. In your experience, have you discovered that most homeless people are also dealing with a mental illness of some sort? If so, is one kind of mental illness more prominent than others?
Kerry Barbieri
Niagara Falls, Ontario
Dear Kerry,
Mental illness is often misunderstood in our society, and this is particularly true as it pertains to people who are homeless or street-involved. It can sometimes be challenging to determine how many homeless people have mental health issues and what types or substance use issues because of the lack of research and data. It is also a challenge to determine whether the mental health issue or substance use caused the person to enter homelessness, or whether these issues arose from their experience of being homeless.
In 2007, the Canadian Institute for Health Information published “Mental Health and Homelessness” report that outlined a number of studies on mental health. There was some general information, but they mainly focused on Post-Traumatic Stress Disorder (PTSD), schizophrenia, substance use and depression. Studies have found that as many as 29% of shelter users have met criteria for one of several mental illnesses including: anti-social personality disorder (along with depression), PTSD or psychotic disorder.
Post-Traumatic Stress Disorder: The same report drew attention to research of homeless youth that found 24% of youth met the criteria for PTSD. Additionally, 40% of youth who met the criteria for Substance Use Disorder also met the criteria for PTSD.
Schizophrenia: There are also overlaps with schizophrenia. One study in Toronto of 300 shelter users found 6% had a psychotic disorder (including schizophrenia). Another study with 124 shelter users in Vancouver found that 7 out of 124 shelter users (nearly 6%) had schizophrenia. This is a significant increase when compared to the general population diagnosis rate of 1%. Substance Use – Throughout Canada, the well-being survey found that 1 to 4% of Canadians have suffered from issues with substance dependence. Several studies have looked at substance dependence and homelessness. A study in Toronto found 68% of shelter users reported a diagnosis of dependence sometime in their life. A study in Vancouver found 44% of homeless adults used non-prescription drugs in the past month. A study in Edmonton found 55% of youth had reported using at least one of the following four drugs in the past year: cocaine, heroin, amphetamines or tranquilizers.
Depression: Throughout Canada, 14-17% of women and 7-10% of men have been diagnosed with depression. In a study conducted in Ottawa, 39% of male youth experiencing homelessness reported symptoms of depression, compared with 20% of male youth who are housed. A separate study, also conducted in Ottawa, found 33% of adult males experiencing homelessness reported having difficulties with mental health; 20% had depression.
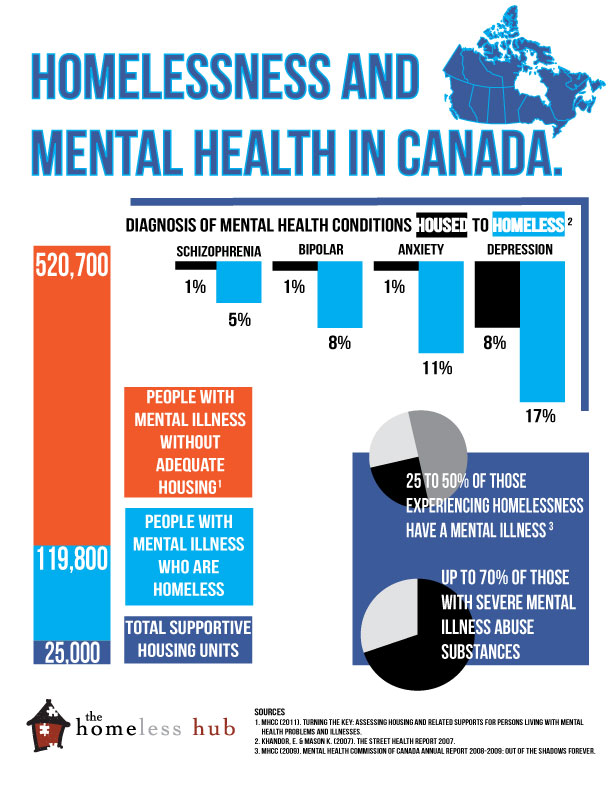
The Mental Health Commission of Canada (MHCC) estimates that between 25 to 50% of homeless people in Canada have mental illness. Out of those with severe mental illness, up to 70% also have difficulty with substance abuse.
MHCC also found that 520,700 people with mental illness are inadequately housed and up to 119,800 people with mental illness are experiencing homeless. Despite these high numbers, there are only 25,000 supportive housing units currently available across Canada.
The interim report (Sept 2012) from the At Home/Chez Soi project administered by MHCC states: “Over 900 individuals from our shelters and on our streets who have not been well served by our current approach are now housed in adequate, affordable and suitable settings. Eighty six percent of participants remain in their first or second unit (as of August 2012). At 12 months those in the Housing First intervention had spent an average of 73% of their time in stable housing. In contrast, those in treatment as usual (TAU) spend only 30% of their time in stable housing. This creates the possibility of better long term health and social functioning outcomes for individuals who have histories of trauma and poor health. Once housed many are beginning to take advantage of the safer places and the opportunities that are created to make better life choices – including pursing opportunities to engage in part or full-time employment.”
As you can see Kerry, it’s hard to get an exact fix on the numbers. What the research does tell us is that there is a strong link between homelessness or insecure housing and mental health issues. Certainly, research has proven that a Housing First approach to solving homelessness – no matter what an individual’s issues are – allows a person to stay housed and to address their other issues over time.
Tanya Gulliver & Isaac Coplan
Homeless Hub
For more information on the relationship between homelessness and mental health visit our Topic – Mental Health.
